
Co-design Future Things for Parkinson’s

- Written byMaria Li
- Published date 06 October 2022

UAL’s Post-Grad Community, in collaboration with Wellcome / EPSRC Centre for Interventional and Surgical Sciences (WEISS), have launched SURGE II: a project bringing together scientists, artists, and the public to explore the complexities and application of technology in surgery.
Maria Li, MA Biodesign (Central Saint Martins) updates us on her SURGE II project with UCL's Dr. Biswajoy Bagchi.
A cross-over between Healthcare Technology and Design
The collaboration with University College London’s Wellcome / EPSRC Centre for Interventional and Surgical Sciences (WEISS) research fellow Dr. Biswajoy Bagchi starts from a matchmaking event held at the Centre’s location in Charles Bell House. I found Biswajoy’s research on Triboelectric Nanogenerators (TENGs) particularly interesting. By tapping the tiny composite TENG pad, one can generate electricity to light up LEDs and the TENGs can also serve as a biocompatible miniature sensor. In the conversation with Biswajoy, we both want to explore different possibilities of this technology, especially in biomedical and surgical applications. We wonder ‘how might we translate this novel health technology into interventional products that fit the needs of the intended users?’ This becomes the driving question for the partnership between Biswajoy and I.
Process
To begin with, we identified patient groups centred around the musculoskeletal remit of healthcare such as patients living with Parkinson’s Disease. From there we started to research online to learn about the common daily challenges faced by patients living with Parkinson’s. We discovered a repeating topic that emerges from the Parkinson’s community, in which the importance of emotional and mental well-being support of patients, as well as carers, is often underestimated. Therefore, we wonder “How might we improve the physical and mental well-being of patients with musculoskeletal diseases in the context of the new TENGs technology?” With this question in mind, we investigated the process of the existing clinical test that assesses patients’ conditions to see if there are any pain points or limitations that needed to be addressed
A Game to Monitor Tremors in Patients with Parkinson's Disease
From our preliminary research, we found the existing tapping test to monitor tremor in patients with Parkinson’s disease often requires patients to travel to the clinic and perform the assessment. The evaluation either solely relies on the clinician’s observation to judge the severity of Parkinsonian motor symptoms according to clinical scales, or patients need to wear a bulky sensor at their fingertips. However, the clinicians’ judgments are inconsistent because of differences in clinical experiences and the weight of the sensor can affect patients’ actions. The clinical setting can also be stressful for patients as they find it difficult to complete the tasks that were asked to do. Seeing these limitations, we wonder if we could apply the TENG sensor here to make the evaluation test more accurate and engaging in order to facilitate self-management to keep track of more accurate monitoring data and potentially help clinicians to offer more personalized treatment. Therefore, we came up with the idea of designing a game that monitors tremors in Patients with Parkinson's Disease.
The first version of the game consists of 3 mini-games measuring fine motor control, and reaction response to visual and audio clues. Participants can play the game individually or with other players.
The responses from participants are recorded via Labview during the game. At the end of the game, the data collected will be analyzed on MATLAB and presented to the participant individually by WEISS researchers.
Here is a video demonstrating the first trial of the tapping game.
Below are some screenshots of the game and the data analysis.


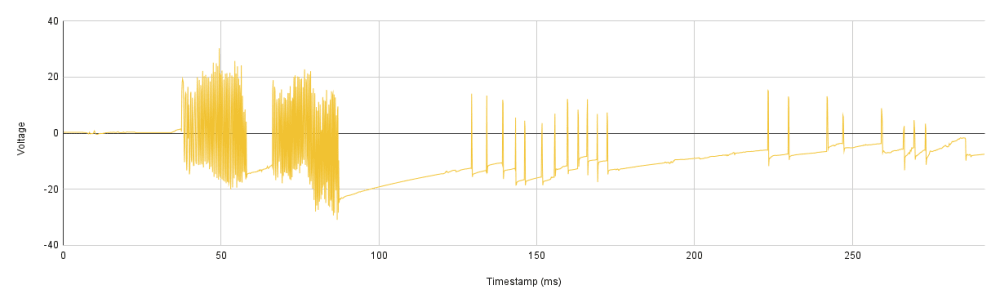
In addition to the game, we also want to explore different ways to visualise the monitoring data. By visualising Parkinson’s condition monitoring data in form of a unique textural landscape generated from the data collected for each patient, we wish to explore a broader view of the perception and understanding of the usefulness of self-monitoring among patients and their families.

Co-design Workshop
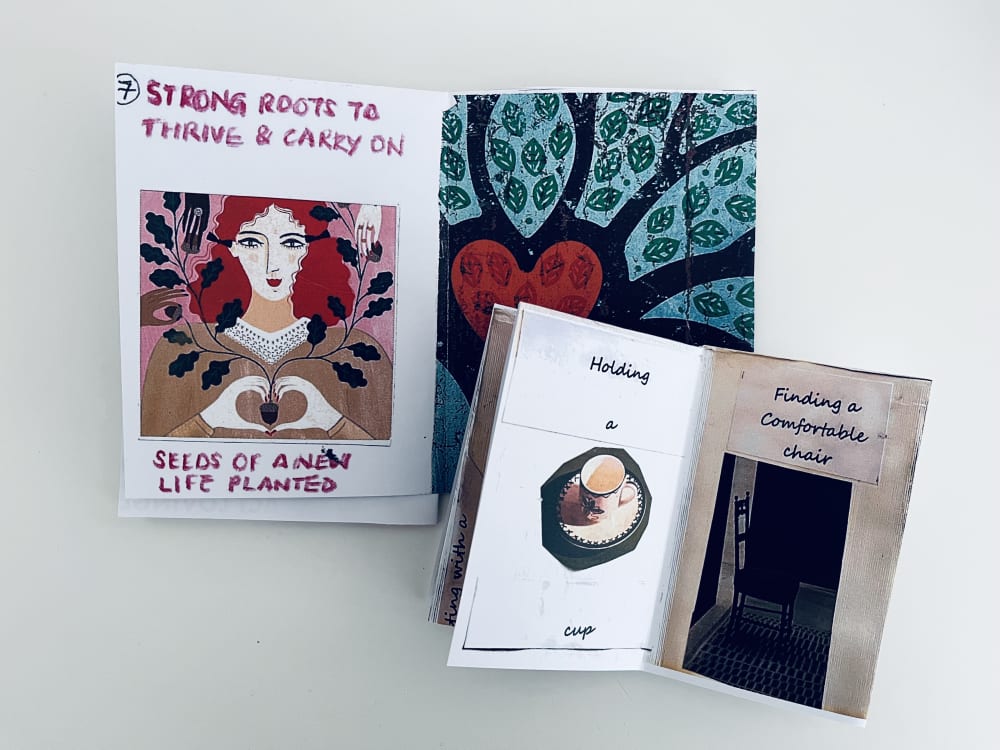
We believe inclusivity and transparency are essential to good research practice for healthcare technologies. We therefore engage patients and carers in the research development through a co-design workshop. There were 3 researchers and 6 public participants with a good mix of patients with Parkinson’s disease and their carers joining online around the UK. In the workshop, both patients and carers shared experiences, and reflected upon the challenges of living with Parkinson’s through zine-making and storytelling. We also demonstrated the interactive game and prompted a discussion about how this new technology could support their daily lives in different scenarios.


The feedback we collected is insightful. We found that communication and transparency in healthcare research are one of the big concerns for patients and their families.
“I don’t know why I need to do the tapping during the clinical assessment.” - Patient with Parkinson’s.
“ If they (the progression) catch it early, you can treat it better. We don't have anything, any knowledge of that.” - Carer
Besides, the socio-cultural background, individual differences among patients, and their mental well-being also require more attention.
“I found some healthcare staff does not understand why my mom (Patient) needs to do things in a certain way (because of cultural practice). We just find it difficult to tell the healthcare staff what exactly happens to my mom’s Parkinson’s in our daily lives” - Carer
“I think it's most important to consult Parkinson's patients because we want to be in charge of our condition.” - Patient with Parkinson’s
“My husband feels very frustrated when he cannot do what the clinician asks him to do in the clinical test.” - Carer
“My dad needs to stop doing things that he loved to do and need to rely on others’ help. This makes him anxious and frustrated as he used to be a very capable man.” - Carer
These findings are valuable for us to identify future directions in designing better healthcare interventions to support people living with Parkinson’s.

Future Development
The next stage of the research involved translating the insights learned from the patients and carers into the design of the interactive supporting platform for Parkinson’s. We identify a few directions for the future direction of research and development:
(i) Increase transparency by informing the patients of how the collected data are interpreted and processes employed to secure data
(ii) Facilitate well-being support for patients with Parkinson’s. For example, adding colour meditation elements into the game to help patients stay relaxed or include social interactions in the game to facilitate communication and gain understanding between patients and their families and friends.
(iii) Enable personalization by allowing patients to customise the level of difficulty of the task to cater to different conditions
In the following iterations, the game aims to enable patients to monitor their Parkinson’s progress comfortably at home and serves as an intervention that encourages patients to stay active and increases the capability to self-management.
Related links
- Find out more about SURGE II
- Wellcome / EPSRC Centre for Interventional and Surgical Sciences (WEISS)
- Follow Maria on Instagram
- View Maria's website
- UAL Post-Grad Community
- SURGE I exhibition walkthrough
UAL Post-Grad Community
Established in 2013, Post-Grad Community is an inclusive platform for all UAL postgraduate students to share work, find opportunities and connect with other creatives within the UAL and beyond. Find out more